Have you ever seen your loved ones gradually turn into a stranger losing all memories of their former self, friends and family? Dementia can do that, and the result may be worse than death.
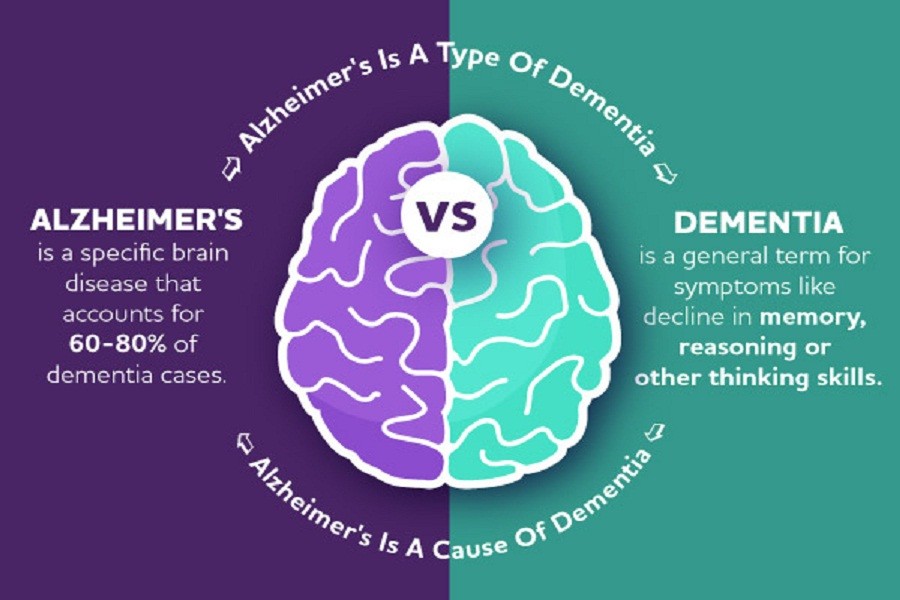
Dementia is basically an umbrella term indicating a chronic progressive condition of deteriorating memory, thinking, and reasoning process. The decline is more than what is expected as a consequence of natural ageing, and significantly limits a person’s ability to function.
Dementia can affect many high-level functions of the brain, including orientation, learning, language, comprehension, judgement, etc. while it commonly affects older people over 65, in about 9.0 per cent of cases, the onset is earlier.
Dementia is a huge public health issue. WHO estimates put the total number of patients worldwide at 55 million, with 60 per cent in low- and middle-income countries like ours. Every year, at least 10 million new cases are added. It is one of the major causes of death and disability in elderly people.
Dementia can manifest in many forms. The most common is Alzheimer’s disease. In addition, it can be due to vascular causes, brain diseases, infections, alcohol or drug abuse, trauma to the head or even nutritional deficiency.
There are many risk factors. Age, depression, social isolation, low educational attainment, and pollution - all are identified as risks. Having a family member with Alzheimer’s also increases the risk for posterity.
There is no treatment for this condition. Physicians may prescribe medications to control the decline, but these are mostly designed for Alzheimer’s and have shown limited effectiveness.
Lifestyle modification can reduce the rate of decline. This includes physical exercise, a healthy and balanced diet, maintaining a good BMI, avoidance of smoking and alcohol, etc. If the patient has other diseases, e.g., hypertension, diabetes, etc. then keeping blood pressure, cholesterol, and sugar levels below the danger level are required.
One of the major impacts of dementia is on family and friends. These patients gradually lose the ability to lead their daily lives, even forgetting how to eat, dress or follow general hygiene.
So, they require a high level of care. Even in a social structure like ours, it is difficult since the 24-hour care of dementia patients is overwhelming and requires training and awareness of the caregivers.
The caregivers are sometimes called the ‘invisible second patient’ in dementia. They suffer from extreme emotional, physical, and sometimes financial stress. This could lead to physical and mental illness, money issues, social isolation, etc.
Any family with a single dementia patient has to go through a serious struggle. They have to watch their loved ones slowly fade into obscurity, being replaced by a stranger.
The patient, in the advanced stage, cannot even recognise his/her own children, husband/wife, the surroundings and often forget where they live. If they get out of the house, they may wander away and could not return.
The whole family needs to come together for providing support. A regular check-up with the physician is mandatory and it must be ensured that the patient is taking the medication as recommended.
Sometimes the best way to do it is to institutionalise the patient. In some countries like ours, there may be some social resistance against it. But this is what’s best for the patient and the family.